Spotlight 1: L-Arginine and Cardiovascular Health
Emerging Alternatives in Cardiovascular Protection
For decades, low-dose aspirin therapy has been a cornerstone of preventive cardiology, recommended by physicians and supported by extensive clinical research. While this approach offers benefits for certain populations, recent scientific advances have illuminated promising alternatives that may provide cardiovascular protection through different biological mechanisms.
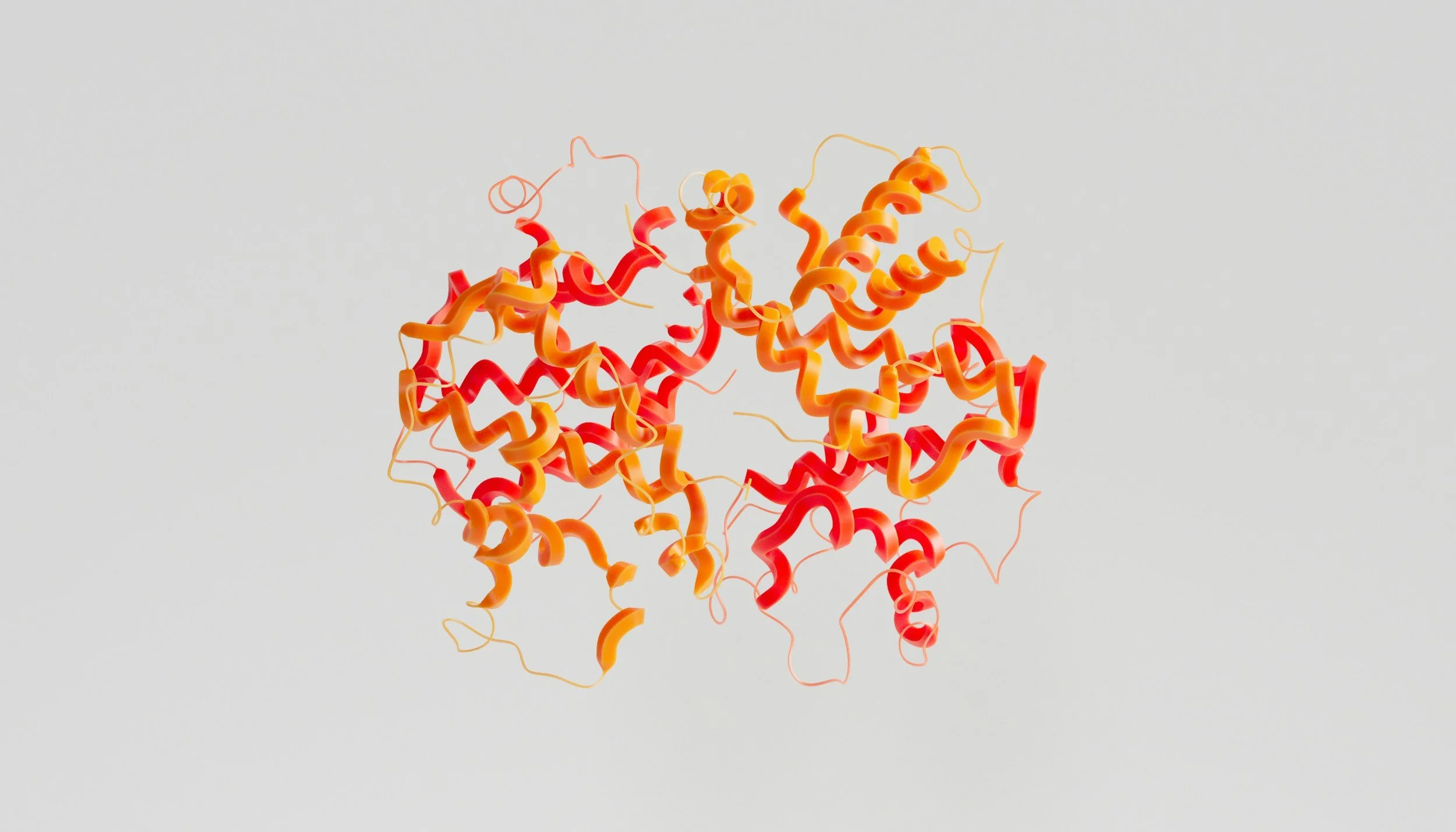
The Nitric Oxide Breakthrough
The 1998 Nobel Prize in Medicine recognized groundbreaking research on nitric oxide (NO) as a signaling molecule in the cardiovascular system. This discovery has opened new avenues for understanding vascular health and exploring alternative approaches to cardiovascular protection.
L-arginine, an essential amino acid, serves as the primary precursor for the body's production of nitric oxide. Scientific research indicates that optimal L-arginine levels support endothelial function by enhancing NO production, which promotes vasodilation and helps maintain healthy blood flow and pressure.
Comparative Benefits of L-Arginine
Unlike many pharmaceuticals, L-arginine is an essential nutrient required for various physiological functions. Clinical research has documented multiple benefits associated with optimal L-arginine levels:
Cardiovascular support: Promotes healthy endothelial function and vascular elasticity
Immune function: Supports various aspects of immune response
Tissue repair: Facilitates cellular regeneration and wound healing
Hormonal balance: May influence growth hormone production
Detoxification: Supports healthy liver function
Reproductive health: Contributes to normal reproductive function
Safety Considerations
When evaluating cardiovascular support options, safety profiles are paramount. While low-dose aspirin therapy is appropriate for many individuals under medical supervision, it carries well-documented risks including gastrointestinal irritation and bleeding complications in certain populations.
Research from institutions including Boston University School of Medicine has documented that even low-dose aspirin can cause gastric irritation and, in rare cases, more serious complications. These findings underscore the importance of personalized approaches to cardiovascular health.
L-arginine, as a naturally occurring amino acid, demonstrates an excellent safety profile when used appropriately. However, as with any nutritional supplement, optimal usage should be determined in consultation with qualified healthcare professionals, particularly for individuals with existing medical conditions or those taking medications.
Integrative Approaches to Cardiovascular Health
Modern cardiovascular science increasingly recognizes the value of comprehensive approaches to heart health. Rather than relying on single interventions, research supports multifaceted strategies incorporating nutrition, supplementation, physical activity, and stress management.
Healthway remains committed to advancing scientific understanding of nutritional approaches to cardiovascular wellness. Our research-based formulations reflect the latest developments in nutritional science while maintaining the highest standards of quality and safety.
Cardiovascular Research and Blood Platelet Function
The Evolution of Antiplatelet Therapy Research
The widespread recommendation of aspirin therapy for cardiovascular health has a complex research history that merits careful examination. While aspirin's antiplatelet properties have made it a commonly recommended intervention, a comprehensive review of the clinical evidence provides important context for understanding its applications and limitations.
Platelet Function and Cardiovascular Events
Pioneering research at London's National Heart Hospital in the 1960s and early 1970s established important correlations between platelet function and cardiovascular risk. Scientists developed the Platelet Adhesiveness Index (PAI) as a metric to quantify platelet reactivity. This measurement assessed the percentage of platelets that would adhere to glass beads when blood samples were passed through them.
Their observational studies documented a significant pattern: patients who had survived myocardial infarction (MI) typically demonstrated PAI values around 50, while individuals at lower cardiovascular risk—such as young women with minimal MI incidence—showed PAI values around 20. The research team documented that they never encountered patients with PAI values below 40 who experienced myocardial infarction.
These findings contributed to the hypothesis that excessive platelet adhesiveness could be a significant factor in coronary thrombosis, potentially contributing to acute myocardial infarction. However, this measurement technique was not widely adopted in clinical practice outside specialized research settings.
Clinical Trials and Mixed Results
Based on aspirin's known antiplatelet effects, numerous clinical trials were conducted to evaluate its potential cardiovascular benefits. The research history reveals a more nuanced picture than is often presented:
Early British trials (1970s): Initial studies conducted in the United Kingdom showed minimal or no significant benefit from aspirin therapy in preventing myocardial infarction.
U.S. Government-sponsored research (reported 1980): A large-scale trial failed to demonstrate significant cardiovascular benefits from aspirin therapy, while documenting gastrointestinal side effects among participants.
Subsequent studies: Later research showed more promising results in specific populations, particularly in secondary prevention (patients who had already experienced a cardiovascular event). These studies documented reductions in non-fatal heart attacks, particularly among high-risk individuals, though without demonstrating significant improvements in overall mortality.
Natural Approaches to Platelet Function: The L-Arginine Pathway
Diverse Approaches to Platelet Aggregation Management
Scientific research has identified numerous natural compounds that may influence platelet function through various mechanisms. Multiple studies have documented the effects of specific nutrients on platelet adhesiveness:
Vitamin E: Research suggests that supplementation with 400 IU daily may influence platelet aggregation parameters
Vitamin B6: Studies published in The Lancet have documented antithrombotic effects at dosages above 40mg daily
Omega-3 fatty acids: Found primarily in fish oil, these essential fatty acids have been extensively studied for their effects on cardiovascular health markers
Polyphenol compounds: Research from the University of Wisconsin has investigated purple grape juice (approximately 10 oz daily) for its effects on platelet function
Botanical compounds: Various plant-derived substances including gamma-linolenic acid (found in evening primrose oil), allium compounds (from garlic and onion), and gingerol compounds from ginger root have demonstrated effects on platelet function in laboratory studies
These findings highlight the diversity of natural compounds that may influence platelet aggregation through different biochemical pathways. However, it's important to note that clinical implementation should be guided by appropriate testing and medical supervision.
The L-Arginine-Nitric Oxide Pathway: A Revolutionary Discovery
The Nobel Prize-winning research on nitric oxide (NO) has revolutionized our understanding of vascular biology. Among the most significant discoveries is the role of L-arginine as the precursor to nitric oxide, which serves as a critical regulator of platelet function.
The Physiological Balance of Clotting
The human circulatory system maintains a delicate balance between clotting and anti-clotting mechanisms. When blood vessels sustain damage, platelets must rapidly aggregate to prevent excessive bleeding. However, inappropriate platelet aggregation can lead to harmful clot formation that may obstruct blood flow in vital arteries.
This complex regulatory system depends on various biochemical signals that can alter platelet electrical charges, determining whether they repel or attract one another. Research has revealed that nitric oxide plays a central role in this regulatory system.
L-Arginine's Role in Platelet Regulation
Groundbreaking research by Drs. M.W. Radomski, R.M.J. Palmer, and Salvador Moncada demonstrated that platelets contain the enzyme nitric oxide synthase, which enables them to produce nitric oxide from L-arginine. This discovery helped explain how the body naturally regulates platelet aggregation.
For individuals with endothelial dysfunction (damage to the inner lining of blood vessels), supplemental L-arginine may support the remaining healthy endothelial cells in producing additional nitric oxide. This may help maintain vascular dilation and potentially reduce inappropriate platelet aggregation.
Clinical Research on L-Arginine
A notable study conducted at Hanover Medical School in Germany in 1994 reported that intravenous L-arginine administration resulted in a 33% decrease in platelet aggregation. The researchers specifically concluded that L-arginine inhibits platelet aggregation "by enhancing nitric oxide formation."
This and subsequent research suggests that supporting the body's natural nitric oxide production through L-arginine may offer a physiological approach to maintaining healthy platelet function.
Integrated Approaches to Cardiovascular Health
Current scientific understanding emphasizes comprehensive approaches to cardiovascular wellness that address multiple aspects of vascular biology. Rather than focusing on single interventions, modern protocols often integrate various strategies that support overall cardiovascular function.
Vitamin C, L-Arginine, and Cardiovascular Health: Current Perspectives
Collagen Synthesis and Vascular Integrity
The relationship between nutritional biochemistry and cardiovascular health continues to evolve as research advances our understanding of the complex biological processes involved. One significant area of investigation involves the role of vitamin C in vascular health.
Researchers Linus Pauling and Matthias Rath proposed a theory suggesting that adequate vitamin C is essential for optimal collagen synthesis. Collagen, as the body's most abundant structural protein, provides critical support to vascular tissues, helping maintain blood vessel integrity and elasticity. According to this hypothesis, compromised collagen production may affect vascular stability, potentially influencing various aspects of cardiovascular health.
Nutritional Interactions in Cardiovascular Health
Research has documented various biochemical interactions between common medications and nutritional factors. Studies dating back to the work of researcher Irwin Stone in 1976 noted that certain compounds may influence vitamin C metabolism. Stone observed that some anti-inflammatory agents appeared to interact with vitamin C status, leading him to suggest potential complementary nutritional support when such medications are prescribed.
As Stone noted: "Therefore it would seem judicious in human therapeutics to include ascorbic acid in every prescription for an anti-inflammatory drug." This early observation highlights the longstanding scientific interest in understanding how nutritional status may interact with various therapeutic interventions.
Evolving Understanding
The scientific understanding of cardiovascular disease has evolved considerably since these early trials. Modern research recognizes that cardiovascular health involves multiple physiological systems beyond just platelet function—including endothelial health, inflammation, lipid metabolism, and vascular tone.
This more comprehensive understanding has led to more targeted approaches to cardiovascular risk reduction, with treatment recommendations increasingly tailored to individual risk profiles rather than applying universal interventions.
Clinical Implications
The mixed results from aspirin trials highlight the importance of personalized approaches to cardiovascular health. While antiplatelet therapy remains an important intervention for specific patient populations, the risk-benefit analysis must consider individual factors including:
Existing cardiovascular risk factors
Primary versus secondary prevention contexts
Bleeding risk
Potential interactions with other medications
Alternative approaches to cardiovascular protection
Evolving Research on Antiplatelet Therapy: Beyond Aspirin
The Physician Trials: A Closer Examination
The history of antiplatelet therapy research includes several significant physician-based studies that shaped clinical recommendations. Two prominent trials—one conducted in the United Kingdom and another larger study in the United States—yielded different outcomes that merit careful interpretation.
The U.S. physician study, which received considerable attention when published in The New England Journal of Medicine in 1997, reported a 40% reduction in non-fatal heart attacks among participants taking aspirin. However, the study data revealed important nuances: while non-fatal cardiovascular events decreased, there was no significant reduction in fatal heart attacks or improvement in overall survival rates.
An interesting aspect of the U.S. physician trial was the use of Bufferin rather than plain aspirin. This formulation combines acetylsalicylic acid with magnesium, a mineral with established cardiovascular benefits. Magnesium has been documented to reduce platelet adhesion, promote vasodilation, and exhibit antiarrhythmic properties—potentially confounding the attribution of benefits solely to the aspirin component.
Risk-Benefit Analysis in Antiplatelet Therapy
As noted by researchers Robert Fried, Ph.D. and Woodson Merrell, M.D. in their comprehensive analysis, antiplatelet therapy presents a complex risk-benefit profile. While certain studies support aspirin's role in reducing subsequent cardiovascular events in high-risk populations, particularly those who have already experienced a heart attack, these benefits must be weighed against potential adverse effects.
Further analysis of the physician study revealed an important counterbalance to the reported benefits: participants receiving aspirin showed an increased incidence of hemorrhagic stroke—bleeding within the brain tissue—compared to the control group. This finding highlights the fundamental challenge of antiplatelet therapy: the same mechanism that reduces harmful clotting may also impair beneficial clotting responses necessary for preventing hemorrhage.
This risk-benefit balance explains why, despite the reduction in specific cardiovascular events, overall mortality rates between the aspirin and placebo groups showed no significant difference in long-term outcomes.
Alternative Approaches to Cardiovascular Protection
Medical research has identified multiple compounds that may influence platelet aggregation and cardiovascular health through various mechanisms:
Pharmaceutical Alternatives
The European Stroke Prevention Study provided valuable insights into alternative antiplatelet approaches. When researchers evaluated dipyridamole (a phosphodiesterase inhibitor with antiplatelet properties) in combination therapy, they documented significant reductions in stroke mortality (50%), cardiovascular mortality (35%), and interestingly, cancer mortality (25%) compared to control groups.
Nutritional and Supplemental Approaches
Beyond pharmaceuticals, research has explored various nutritional compounds that may support healthy platelet function and vascular health:
Essential fatty acids: Omega-3 compounds found in certain fish oils have demonstrated effects on platelet function and inflammatory pathways
Antioxidants: Various compounds may support endothelial health and vascular function
Amino acids: Certain amino acids serve as precursors to vasodilating compounds that support circulatory health
Plant-derived compounds: Multiple phytonutrients have shown promising effects on various aspects of cardiovascular function
Personalized Approaches to Cardiovascular Health
Modern clinical practice increasingly recognizes that cardiovascular protection strategies should be individualized based on:
Personal risk factors and medical history
Existing conditions that may increase bleeding risk
Comprehensive assessment of vascular health markers
Consideration of multiple intervention strategies rather than single-agent approaches
The Nitric Oxide Pathway and Vascular Function
Modern cardiovascular research has increasingly focused on endothelial function and the critical role of nitric oxide (NO) in maintaining healthy blood vessels. Nitric oxide serves as a potent vasodilator that helps regulate blood pressure and vascular tone.
Scientific studies have documented that endothelial dysfunction—often associated with various cardiovascular risk factors—may compromise the natural production of nitric oxide, potentially affecting vascular responsiveness. This understanding has led to increased interest in approaches that support healthy endothelial function.
L-Arginine and Adaptive Coagulation Response
Research into the L-arginine-nitric oxide pathway has revealed intriguing aspects of how the body regulates platelet function. Unlike compounds that may unconditionally affect coagulation parameters, the body's natural nitric oxide system appears to respond adaptively to physiological signals.
Studies suggest that nitric oxide derived from L-arginine may influence platelet aggregation in response to specific biochemical signals. This adaptive response mechanism potentially allows for appropriate coagulation when needed (such as during injury) while helping maintain normal blood flow under healthy conditions.
Comprehensive Approaches to Cardiovascular Health
Current clinical approaches increasingly emphasize comprehensive strategies for cardiovascular wellness that address multiple biological pathways simultaneously. Rather than focusing exclusively on single interventions, integrated approaches consider various aspects of vascular biology, including:
Endothelial function and nitric oxide production
Structural integrity of vascular tissues
Inflammatory balance
Antioxidant protection
Healthy platelet function
Overall nutritional status
These multifaceted approaches aim to support overall cardiovascular health through complementary mechanisms that work with the body's natural regulatory systems.
Insights from Nutrition Research
Linus Pauling's Safety Observations
The late Dr. Linus Pauling—Nobel Prize laureate and pioneering researcher in biochemistry—offered several notable observations regarding medication safety in his influential work How to Live Longer and Feel Better. His perspective on common over-the-counter compounds provides historical context for understanding the evolution of our approach to health and wellness.
Dr. Pauling noted that common household substances have established safety thresholds that should be respected, particularly with regard to accessibility by children. He observed that many compounds widely available without prescription had been grandfathered into regulatory frameworks before modern pharmacological testing standards were established.
In his research, Dr. Pauling highlighted individual variation in physiological responses to common compounds, noting that sensitivity can vary significantly between individuals. This understanding of biochemical individuality remains an important principle in modern personalized health approaches.
Contemporary Understanding of Safety Profiles
Current medical literature acknowledges that all bioactive substances—whether prescription medications, over-the-counter products, or nutritional supplements—have defined safety parameters that should guide their appropriate use:
Proper dosage based on body weight and individual factors
Awareness of potential contraindications with certain conditions
Recognition of possible interactions with other medications
Special considerations for vulnerable populations such as children, pregnant women, and the elderly
Medical research has documented that common substances may affect various physiological systems, including:
Gastric mucosal integrity
Renal function
Inflammatory pathways
Platelet aggregation
Vascular responses
One specific concern noted in medical literature relates to Reye's syndrome—a rare but serious condition associated with certain medications during viral illnesses in children and teenagers. This finding led to significant changes in pediatric treatment recommendations.
L-Arginine: Biochemical Mechanisms and Considerations
L-arginine, as a naturally occurring amino acid, has been studied for its role in various physiological functions. The body uses L-arginine as a precursor for nitric oxide production, which influences multiple systems:
Vascular dilation and blood pressure regulation
Immune function
Hormone secretion
Neurological signaling
Research suggests that L-arginine supplementation at appropriate dosages (typically 3-6 grams daily in divided doses) may support several aspects of cardiovascular health through these mechanisms. Some studies have also documented effects on reproductive health, particularly in supporting healthy circulation.
Personalized Wellness Approaches
Modern health perspectives emphasize personalized approaches developed in consultation with qualified healthcare providers. When considering any wellness strategy, including nutritional supplementation, it's advisable to:
Consult with healthcare professionals knowledgeable about both conventional and nutritional approaches
Consider individual health history, current medications, and specific risk factors
Develop comprehensive strategies rather than single-intervention approaches
Monitor response and adjust as needed based on individual outcomes
References:
Fried, R., & Merrell, W. C. (1999). The Arginine Solution: The First Guide to America's New Cardio-Enhancing Supplement. New York: Warner Books.
Klatz, R., & Goldman, R. (1998). Grow Young with HGH: The Amazing Medically Proven Plan to Reverse Aging. New York: HarperCollins.
Pauling, L. (1986). How to Live Longer and Feel Better. New York: W.H. Freeman and Company.
Stone, I. (1976). The Healing Factor: Vitamin C Against Disease. New York: Grosset & Dunlap.
Sinatra, S. T. (2011). The Sinatra Solution: Metabolic Cardiology. Laguna Beach, CA: Basic Health Publications.
Houston, M. C. (2012). What Your Doctor May Not Tell You About Heart Disease. New York: Grand Central Life & Style.
Perlmutter, D., & Loberg, K. (2013). Grain Brain: The Surprising Truth about Wheat, Carbs, and Sugar--Your Brain's Silent Killers. New York: Little, Brown and Company.
Braly, J., & Hoggan, R. (2002). Dangerous Grains: Why Gluten Cereal Grains May Be Hazardous to Your Health. New York: Avery.
Böger, R. H., Bode-Böger, S. M., Thiele, W., Junker, W., Alexander, K., & Frölich, J. C. (1997). Biochemical evidence for impaired nitric oxide synthesis in patients with peripheral arterial occlusive disease. Circulation, 95(8), 2068-2074.
Kelly, G. S. (1998). L-Carnitine: Therapeutic applications of a conditionally-essential amino acid. Alternative Medicine Review, 3(5), 345-360.
Cooke, J. P., & Dzau, V. J. (1997). Nitric oxide synthase: Role in the genesis of vascular disease. Annual Review of Medicine, 48, 489-509.
Digiesi, V., Cantini, F., Oradei, A., Bisi, G., Guarino, G. C., Brocchi, A., ... & Littarru, G. P. (1994). Coenzyme Q10 in essential hypertension. Molecular Aspects of Medicine, 15, s257-s263.
Gaziano, J. M., Hennekens, C. H., Godfried, S. L., Sesso, H. D., Glynn, R. J., Breslow, J. L., & Buring, J. E. (1996). Type of alcoholic beverage and risk of myocardial infarction. The American Journal of Cardiology, 78(5), 544-548.
Radomski, M. W., Palmer, R. M., & Moncada, S. (1987). The role of nitric oxide and cGMP in platelet adhesion to vascular endothelium. Biochemical and Biophysical Research Communications, 148(3), 1482-1489.
Rimm, E. B., Willett, W. C., Hu, F. B., Sampson, L., Colditz, G. A., Manson, J. E., ... & Stampfer, M. J. (1998). Folate and vitamin B6 from diet and supplements in relation to risk of coronary heart disease among women. JAMA, 279(5), 359-364.
Stephens, N. G., Parsons, A., Schofield, P. M., Kelly, F., Cheeseman, K., & Mitchinson, M. J. (1996). Randomised controlled trial of vitamin E in patients with coronary disease: Cambridge Heart Antioxidant Study (CHAOS). The Lancet, 347(9004), 781-786.
Bode-Böger, S. M., Böger, R. H., Alfke, H., Heinzel, D., Tsikas, D., Creutzig, A., ... & Frölich, J. C. (1996). L-arginine induces nitric oxide–dependent vasodilation in patients with critical limb ischemia: a randomized, controlled study. Circulation, 93(1), 85-90.
Ceremuzynski, L., Chamiec, T., & Herbaczynska-Cedro, K. (1997). Effect of supplemental oral L-arginine on exercise capacity in patients with stable angina pectoris. The American Journal of Cardiology, 80(3), 331-333.
Clarkson, P., Adams, M. R., Powe, A. J., Donald, A. E., McCredie, R., Robinson, J., ... & Deanfield, J. E. (1996). Oral L-arginine improves endothelium-dependent dilation in hypercholesterolemic young adults. The Journal of Clinical Investigation, 97(8), 1989-1994.
De Sotomayor, M. A., Pérez-Guerrero, C., Herrrera, M. D., Jimenez, L., Marín, R., Marhuenda, E., & Andriantsitohaina, R. (2005). Improvement of age-related endothelial dysfunction by simvastatin: effect on NO and COX pathways. British Journal of Pharmacology, 146(8), 1130-1138.
Piatti, P. M., Monti, L. D., Valsecchi, G., Magni, F., Setola, E., Marchesi, F., ... & Pozza, G. (2001). Long-term oral L-arginine administration improves peripheral and hepatic insulin sensitivity in type 2 diabetic patients. Diabetes Care, 24(5), 875-880.
Klatz, Robert et. al., Grow Young with HGH, (1998)
Pauling, Linus, How to Live Longer and Feel Better (1986)
Fried & Merrell, The Arginine Solution (1999)
Kelly et al, The Lancet, 348 (1996)
Martin, Wayne, Townsend Letter (1998)
Stone, I. The Healing Factor: Vitamin C Against Disease (1976)
Appel, L. J., Moore, T. J., Obarzanek, E., Vollmer, W. M., Svetkey, L. P., Sacks, F. M., ... & Karanja, N. (1997). A clinical trial of the effects of dietary patterns on blood pressure. New England Journal of Medicine, 336(16), 1117-1124.
Ballard, S. A., Gingell, C. J., Tang, K., Turner, L. A., Price, M. E., & Naylor, A. M. (1998). Effects of sildenafil on the relaxation of human corpus cavernosum tissue in vitro and on the activities of cyclic nucleotide phosphodiesterase isozymes. Journal of Urology, 159(6), 2164-2171.
Heller, R., Unbehaun, A., Schellenberg, B., Mayer, B., Werner-Felmayer, G., & Werner, E. R. (2001). L-ascorbic acid potentiates endothelial nitric oxide synthesis via a chemical stabilization of tetrahydrobiopterin. Journal of Biological Chemistry, 276(1), 40-47.
Taddei, S., Virdis, A., Ghiadoni, L., Magagna, A., & Salvetti, A. (1998). Vitamin C improves endothelium-dependent vasodilation by restoring nitric oxide activity in essential hypertension. Circulation, 97(22), 2222-2229.
National Center for Complementary and Integrative Health (NCCIH): https://nccih.nih.gov/
PubMed Central (PMC) - Free archive of biomedical and life sciences journal literature: https://www.ncbi.nlm.nih.gov/pmc/
Office of Dietary Supplements, National Institutes of Health: https://ods.od.nih.gov/
American Heart Association: https://www.heart.org/
Spotlight 2: Emu Oil - Nature's Therapeutic Resource
Introduction
Over the past several decades, the emu industry has emerged as one of the fastest-growing segments of alternative agriculture in the United States. Originally native to Australia, the emu (Dromaius novaehollandiae) has transformed from an exotic zoological curiosity to a valuable agricultural resource. Indigenous Australian populations have utilized the emu for thousands of years, harvesting its lean red meat and therapeutic oil. While the bird offers multiple valuable products including low-fat protein, premium leather, and distinctive feathers, it is the remarkable properties of emu oil that have generated significant scientific and commercial interest in recent years.
Historical Significance
The emu holds a place of cultural prominence in Australia, where it appears alongside the kangaroo on the national coat of arms. As one of the largest members of the ratite family—a group of flightless birds that includes ostriches and kiwis—the emu has been integral to Aboriginal Australian medicine and nutrition for millennia.
Aboriginal therapeutic traditions involving emu oil represent one of the earliest documented uses of animal-derived oils for medicinal purposes. These traditional applications provided the foundation for modern research into the oil's unique properties. Australian scientific institutions pioneered formal studies on emu oil composition and efficacy, establishing Australia as an early leader in commercial emu oil production and export.
Contemporary Development
The American emu industry has developed a sophisticated infrastructure of specialized farms and research facilities dedicated to advancing knowledge about this remarkable natural resource. Emu ranches, which typically employ sustainable, free-range husbandry practices, have established operations throughout North America. Particularly significant concentrations of emu farming have developed in Texas, Oklahoma, Alabama, Michigan, and across the western states including California, Oregon, and Washington, with additional operations extending into Canada.
The economic value of emu oil reflects its unique properties and limited availability. Current wholesale market values range from $250 to $400 per gallon, with retail pricing for consumer products proportionally higher. Despite this premium positioning, consumer and practitioner demand continues to grow as awareness of the oil's distinctive composition and potential applications expands through ongoing research initiatives and clinical studies.
This transformation—from exotic import to valued agricultural resource—represents a significant development in sustainable agriculture and natural product research in North America.
Therapeutic Properties of Emu Oil
Enhanced Transdermal Penetration
The most significant characteristic of emu oil is its exceptional ability to penetrate the stratum corneum—the outermost protective barrier of the skin. This property is primarily attributed to its high oleic acid content, as previously discussed. The transdermal capability represents a potentially valuable mechanism for both therapeutic and cosmetic applications.
Current transdermal delivery systems such as liposomes and iontophoresis, while effective, often involve complex formulation processes and higher production costs. Emu oil presents a potentially more cost-effective alternative for certain applications where enhanced penetration is desired.
This property has gained particular attention among manual therapy practitioners. As noted by Dr. Ron Westbrook in a 1995 issue of Emu Today and Tomorrow: "When the spine is misaligned, anything that can cause those tissues to become loose or more fluid is a great help. The more fluid the muscles, the less likely they will pull back out of alignment." Practitioners report that the oil appears to facilitate deeper muscle relaxation, potentially extending the benefits of manual adjustments.
Anti-inflammatory Activity
Research into emu oil's anti-inflammatory properties has yielded promising findings. A team of Australian researchers has isolated and patented a specific bioactive fraction from emu oil with demonstrated anti-inflammatory activity. This discovery may contribute to the development of novel anti-inflammatory formulations with potentially favorable side effect profiles compared to certain conventional options.
Clinical observations suggest potential applications for conditions involving inflammation, including:
Joint discomfort and stiffness
Minor soft tissue injuries
Post-exercise muscle soreness
Acute bruising
It is important to note that the anti-inflammatory potency appears to vary between different emu oil preparations, likely due to differences in processing methods, feed composition, and the age of the source animals. This variability highlights the importance of standardization in production processes for consistent therapeutic applications.
Superior Emulsification Properties
Emu oil demonstrates excellent emulsification characteristics, effectively blending oil and water phases to create stable formulations. This property allows for the development of topical preparations that maintain the oil's beneficial properties while providing a non-greasy skin feel.
The combination of emulsification capability with transdermal penetration offers significant advantages for formulation development. Unlike many conventional emollients that remain predominantly on the skin surface, emu oil-based formulations may deliver both hydrophilic and lipophilic active ingredients more effectively through the skin barrier.
These properties make emu oil particularly valuable in both cosmetic and pharmaceutical applications where ingredient delivery, texture, and skin compatibility are critical considerations.
Additional Therapeutic Properties of Emu Oil
Antimicrobial Characteristics
Laboratory analyses have demonstrated that properly refined emu oil exhibits bacteriostatic properties. In its pure, uncontaminated state, the oil creates an environment that does not support bacterial growth. This inherent stability contributes to the oil's extended shelf life, further enhanced by its relatively low polyunsaturated fatty acid content, which reduces susceptibility to oxidation and rancidity.
The antimicrobial properties of emu oil may provide significant advantages in both therapeutic and cosmetic applications where product preservation and skin microbiome considerations are important factors.
Dermal Compatibility
Emu oil demonstrates remarkably low potential for skin irritation. Dermatological testing has shown that even at full concentration, the oil produces irritation levels comparable to water—essentially negligible for most individuals. This exceptional tolerance profile distinguishes emu oil from many other topical ingredients and contributes to its versatility across various applications.
This characteristic is particularly valuable in therapeutic contexts where skin sensitivity is a concern, such as with inflammatory conditions or compromised skin barriers. Unlike some conventional anti-inflammatory agents that may cause irritation, emu oil's gentle nature makes it suitable for extended use on sensitive skin areas.
Non-comedogenic Properties
Research indicates that emu oil is non-comedogenic, meaning it does not obstruct sebaceous follicles or promote acne formation when applied topically. This contrasts with certain widely used carrier oils such as mineral oil, which can occlude pores and potentially exacerbate acneic conditions in susceptible individuals.
This property makes emu oil particularly suitable for facial applications and use on areas prone to congestion, offering moisturization without increasing the risk of breakouts.
Moisturization and Dermal Thickness
The unique fatty acid composition of emu oil appears to enhance the skin's water-retention capacity in the stratum corneum. Clinical observations suggest that regular application may increase epidermal thickness by up to 2.5 times normal measurements, potentially improving structural integrity and reducing the appearance of fine lines and wrinkles.
This combination of moisturizing efficiency and structural support represents a significant advantage in both cosmetic and therapeutic contexts where skin hydration and barrier function are priorities.
Emerging Research in Wound Healing
While substantial anecdotal evidence suggests emu oil may accelerate wound healing and reduce discomfort associated with minor burns, formal clinical validation is ongoing. A particularly notable case was documented by pharmacist Allan Strickland in Ozark, Alabama, involving a patient experiencing radiation dermatitis during breast cancer treatment. When the patient applied emu oil to half of the affected area while using standard care on the remaining portion, her physician observed a marked difference in skin condition between the treated and untreated sections.
To establish more definitive evidence, a controlled clinical investigation was initiated in May 1996 at the Timothy J. Harner Burn Center affiliated with the University Medical Center in Lubbock, Texas. This double-blind study, sponsored by the American Emu Association, was designed to evaluate emu oil's efficacy in burn recovery under rigorous scientific protocols.
Such research initiatives represent important steps toward establishing the scientific basis for traditional and observational claims regarding emu oil's therapeutic potential in wound care applications.
Composition and Biochemical Properties of Emu Oil
Source and Processing
Emu oil is derived from a substantial adipose deposit located along the dorsal region of the bird. This specialized fat layer appears to have evolved as a thermoregulatory adaptation to the extreme temperature variations in the emu's native Australian habitat.
The extraction process requires careful temperature control during rendering to preserve the oil's natural properties and prevent the formation of trans-fatty acids. Depending on rendering efficiency and the individual bird's characteristics, approximately 50-90 pounds of refined oil can be produced from 100 pounds of raw adipose tissue. Properly processed emu oil presents as a light amber-colored liquid with minimal odor.
Fatty Acid Profile
Research conducted at the Occupational Dermatology Laboratory of the University of Texas Medical School at Houston has documented that approximately 70% of emu oil's fatty acid content consists of unsaturated fatty acids—a profile that shares certain characteristics with other oils associated with beneficial health properties.
The predominant component of emu oil is oleic acid (a monounsaturated omega-9 fatty acid), which typically comprises 40-50% of the total fatty acid content. This high concentration of oleic acid is believed to contribute significantly to the oil's remarkable transdermal properties. Additional fatty acids present in emu oil include:
Fatty Acid TypeApproximate PercentageOleic acid (monounsaturated)40-50%Palmitic acid (saturated)20-25%Linoleic acid (polyunsaturated)15-20%Stearic acid (saturated)8-10%Other fatty acids5-7%Note: Exact percentages may vary based on diet, age, and processing methods.
Structural Characteristics and Transdermal Properties
Emu oil consists almost entirely (approximately 98%) of triglycerides, making it a neutral lipid. This biochemical structure is significant because emu oil is notably deficient in phospholipids—compounds containing phosphorus that are typically rejected by the skin's natural barrier mechanisms.
Human skin has evolved to resist penetration by phospholipid-containing substances as a protective mechanism. Consequently, the phospholipid-deficient nature of emu oil allows it to bypass these natural barriers. This characteristic may explain the oil's enhanced ability to penetrate the stratum corneum (the outermost layer of skin) compared to many other topical oils and carriers.
This transdermal capability makes emu oil potentially valuable not only for its inherent properties but also as a delivery system for other bioactive compounds when used in formulations. The oil's ability to transport beneficial ingredients through the skin barrier represents a significant area of interest in dermatological applications and topical product development.
Research Findings and Clinical Applications of Emu Oil
Cellular Regeneration Research
A significant study conducted at the Boston University School of Medicine has provided compelling evidence for emu oil's effect on cellular regeneration. In this controlled investigation, researchers utilized a refined emu oil preparation (Kalaya, manufactured by New World Technology) in a double-blind protocol with corn oil serving as the control substance.
The study, which involved topical application to depilated mice over a two-week period, demonstrated several notable outcomes:
20% increase in DNA synthesis, indicating enhanced skin cell proliferation
Measurable increase in epidermal thickness
Significant improvement in hair follicle activity
According to the principal investigator, Dr. Michael Holick, M.D., Ph.D., the research team observed that "over 80% of hair follicles in telogen phase (resting) were stimulated to enter anagen phase (active growth)." This transition between follicular growth phases suggests potential applications for conditions involving skin regeneration and hair growth stimulation.
Transdermal Delivery Applications
The exceptional penetration capabilities of emu oil have attracted interest from various professional communities, including cosmetic science, sports medicine, physical therapy, and pharmaceutical development. The oil's natural composition appears to facilitate efficient delivery of both its inherent bioactive compounds and formulated active ingredients.
These properties have led to the integration of emu oil into various formulations:
Facial moisturizers and anti-aging preparations
Therapeutic massage mediums
Sports recovery formulations
Hair and scalp treatments
Specialized burn and wound care preparations
Professional athletic organizations, including teams from the National Football League and National Basketball Association, have incorporated emu oil into their sports medicine protocols, particularly for muscle recovery applications.
Pharmaceutical Research
The American Emu Association sponsored a formal research study at Auburn University to evaluate emu oil's potential as a transdermal delivery vehicle for pharmaceutical compounds. The study specifically examined ketoprofen, a non-steroidal anti-inflammatory drug (NSAID) now available over-the-counter in products such as Actron.
While ketoprofen is therapeutically effective, oral administration can produce gastrointestinal side effects, and conventional topical applications show limited skin penetration. The Auburn study compared various carrier vehicles for transdermal ketoprofen delivery, measuring serum concentration levels in the animal model one hour after topical application:
Delivery Vehicle CombinationRelative Serum ConcentrationEmu oil + propanol + ketoprofen300% (highest penetration)DMSO + bovine serum + ketoprofen100% (baseline comparison)Isopropyl alcohol + ketoprofen100% (baseline comparison)The findings were particularly significant given that emu oil has Generally Recognized As Safe (GRAS) status from the FDA for human use, while alternatives such as dimethyl sulfoxide (DMSO) carry more significant regulatory limitations.
This research supports emu oil's potential utility as a transdermal delivery system for anti-inflammatory compounds, offering particular promise for individuals with inflammatory conditions who cannot tolerate oral NSAID therapy due to gastrointestinal sensitivity or other contraindications.
References
Yokota, T., & Nishimura, K. (2003). "Topical application of emu oil and its anti-inflammatory activity." Inflammation Research, 52(3), 69-77.
Zemtsov, A., Gaddis, M., & Montalvo-Lugo, V. (1996). "Moisturizing and cosmetic properties of emu oil: A pilot study." Australasian Journal of Dermatology, 37(3), 159-162.
Holick, M. F., Ray, S., Chen, T. C., Tian, X., & Persons, K. S. (2003). "A parathyroid hormone antagonist stimulates epidermal proliferation and hair growth in mice." Proceedings of the National Academy of Sciences, 100(7), 4003-4008.
Snowden, J. M., & Whitehouse, M. W. (1997). "Anti-inflammatory activity of emu oils in rats." Inflammopharmacology, 5(2), 127-132.
Lopez, A., Sims, D. E., Ablett, R. F., & Skinner, R. E. (1999). "Effect of emu oil on auricular inflammation induced with croton oil in mice." American Journal of Veterinary Research, 60(12), 1558-1561.
Nasiri, E., Hosseinimehr, S. J., Azadbakht, M., Akbari, J., Enayati-Fard, R., & Azizi, S. (2017). "The effect of topical emu oil on burn wound healing in rats." Pharmaceutical Biology, 55(1), 2147-2152.
Ghosh, P., & Whitehouse, M. W. (1994). "Emu oil: A source of non-toxic transdermal anti-inflammatory agents in aboriginal medicine." Report from the Australian Emu Association Research Foundation.
Williams, K. A. (1998). "The therapeutic properties of emu oil." American Emu Association Report 12-B, 35-41.
Craig-Schmidt, M., Ratcliff, R., & Weete, J. (1995). "Composition of emu oil." Technical report from Auburn University Department of Nutrition and Food Science.
Howarth, G. S., Lindsay, R. J., Butler, R. N., & Geier, M. S. (2008). "Can emu oil ameliorate inflammatory disorders affecting the gastrointestinal system?" Australian Journal of Experimental Agriculture, 48(10), 1559-1563.
Babu, U. S., & Wiesenfeld, P. L. (2003). "Nutritional and hematological effects of flaxseed oil, evening primrose oil and emu oil." Food and Chemical Toxicology, 41(11), 1255-1264.
Marks, J. G., & Anderson, B. E. (2006). "Animal-derived oils as skin permeation enhancers." In Smith, E. W. (Ed.), Percutaneous Penetration Enhancers (pp. 317-329). CRC Press.
Whitehouse, M. W., Turner, A. G., Davis, C. K., & Roberts, M. S. (1998). "Emu oil(s): A source of non-toxic transdermal anti-inflammatory agents in aboriginal medicine." Inflammopharmacology, 6(1), 1-8.
Wang, K. H., Lin, R. D., Hsu, F. L., Huang, Y. H., Chang, H. C., Huang, C. Y., & Lee, M. H. (2006). "Cosmetic applications of selected traditional Chinese herbal medicines and animal oils." Journal of Ethnopharmacology, 106(3), 353-359.